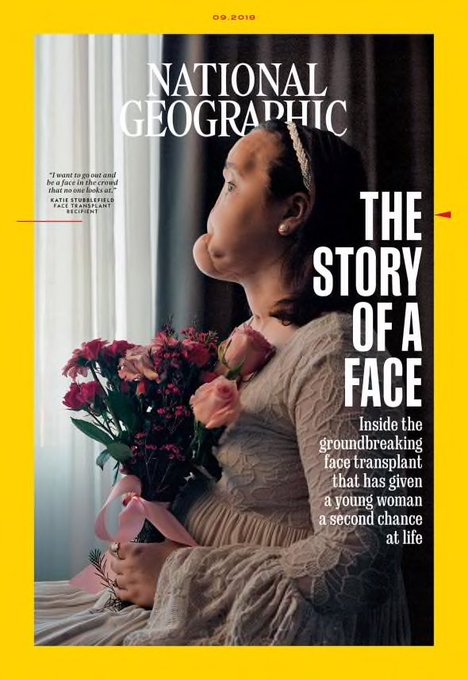
Norte-americana de 22 anos tentou suicidar-se quando tinha 18. Uma cirurgia de 31 horas deu-lhe um novo rosto e uma nova vida. A National Geographic acompanhou-a durante um ano
Quando em 2015, Katie Stubblefield se tentou matar com um tiro no queixo, os médicos conseguiram salvar-lhe a vida, mas não o rosto. Passados quatro anos e 22 cirurgias, a norte-americana, hoje com 22 anos, tornou-se a mais jovem paciente, nos Estados Unidos, a receber um transplante facial. 31 horas e 11 cirurgiões numa clínica em Cleveland, no estado de Ohio, conseguiram mudar a sua história, como conta a edição de setembro da revista National Geographic, que acompanhou a adolescente durante um ano e assistiu à operação.
Katie esteve um ano na lista de espera para o transplante. Em 2017, recebeu a tão aguardada confirmação de que já havia doadora - uma rapariga de 31 anos que morreu com uma overdose. O seu seguro médico é que não cobria as despesas, uma vez que o procedimento médico é considerado experimental. No entanto, segundo a National Geographic, o Instituto de Medicina Regenerativa das Forças Armadas norte-americanas terá comparticipado o transplante, uma vez que tem interesse no aperfeiçoamento da técnica para poder recorrer à mesma em feridos de guerra.
Katie conta na reportagem que ainda sente algumas dificuldades para falar e que ficará para o resto da vida sujeita a tomar medicação para reduzir o risco de o seu organismo rejeitar o transplante. No entanto, a clínica Cleveland, onde é acompanhada depois de ter sido tratada no Mississipi, refere que a operação vai permitir a Katie ter uma "oportunidade para viver uma vida funcional".
"Esta operação vai dar à paciente a capacidade de falar mais claramente e de respirar, mastigar e engolir de forma mais eficiente. Poderá também melhorar as suas expressões faciais. Vai favorecer as suas funções físicas, psicológicas e sociais", pode ler-se no site da clínica.
Katie diz que não se recorda de muita coisa antes da tentativa de suicídio. A família, com quem a revista cientifica também falou, lembra que a adolescente estava a passar por uma fase complicada: lutava com problemas emocionais e de saúde.
A bala destruiu a maior parte do rosto da jovem, incluindo o nariz, a testa e o maxilar. Ficou ainda com lesões no cérebro e nos olhos. Desde que fez o transplante facial, Katie já foi sujeita a três operações de reconstrução e não deve ficar por aqui. A jovem continua a receber ajuda psicológica e já pensa em partilhar a sua experiência com adolescentes com pensamentos suicidas. Os seus planos para o futuro passam por "ajudar outras pessoas" e ir para a faculdade.
Katie Stubblefield foi a 40.º paciente a receber um transplante facial total no mundo, segundo a BBC. O primeiro procedimento deste género foi realizado em Barcelona, em março de 2010. Uma equipa de 30 médicos espanhóis operaram, durante 22 horas, uma pessoa cuja identidade não foi revelada na altura. Só meses mais tarde, Oscar (assim, sem apelido) apareceu em público, ficando a saber-se que se tratava de um agricultor de 31 anos que ficara desfigurado num acidente com armas de fogo.
Nos EUA, a primeira pessoa a receber um transplanta facial total foi Dallas Wiens, um empregado da construção civil operado em 2011, três anos depois de ter sofrido queimaduras muito graves por eletrocussão.


Cleveland Clinic Performs Third Face Transplant
11 surgeons, multiple specialists transplant 100 percent of patient’s facial tissue; patient is youngest in the United States to receive a face transplant
JULY 18, 2017 /
In a 31-hour surgery in May, a team of 11 Cleveland Clinic surgeons and multiple specialists performed the hospital’s third face transplant – and its first total face transplant – on a 21-year-old female who suffered severe facial trauma and other complications from a gunshot wound as a teenager.
The surgery included transplantation of the scalp, the forehead, upper and lower eyelids, eye sockets, nose, upper cheeks, upper jaw and half of lower jaw, upper teeth, lower teeth, partial facial nerves, facial muscles, and skin, effectively replacing 100 percent of the patient’s facial tissue.
“To reach this point of recovery has often times been a difficult road to travel, but I’m thankful there’s been a road – and Cleveland Clinic has been the vehicle to help drive me along,” said the recipient. “I am forever grateful for the care this hospital has given me and continues to offer on my journey of recovery and healing. To call my surgeons, physicians, nurses and caregivers ‘world class’ would be an understatement. And to my donor and her family – words cannot express the appreciation I have for this incredible gift. With a grateful heart, I say ‘thank you’ to all who have made this possible for me.”
To protect the privacy of those involved, no further information will be released about the patient, the donor or their families.
Co-directed by Frank Papay, M.D., chairman of the Dermatology and Plastic Surgery Institute, and Maria Siemionow, M.D., Ph.D., the surgical team included Brian Gastman, M.D.; James Zins, M.D.; Risal Djohan, M.D.; Mark Hendrickson, M.D.; Graham Schwarz, M.D.; Antonio Rampazzo, M.D., Ph.D.; Bahar Bassiri Gharb, M.D., Ph.D.; Raffi Gurunluoglu, M.D.; and Steven Bernard, M.D. Specialists from anesthesia, bioethics, dentistry, immunology, ophthalmology, endocrinology, infectious disease, pharmacy, psychiatry and transplant were also involved.
“Plastic surgery is about restoring form and function,” said Dr. Papay. “Function comes before form, and prior to the face transplant, this patient had extremely poor function and form. Our job in reconstruction is to weigh the risk versus the benefit of doing face transplantation, and we felt the risk was well worth it to give this patient better function, better social form and, ultimately, a better life. Advances in face transplantation are an example of the Cleveland Clinic’s collaborative innovation. We’re much more capable together than we are individually, and I’m extremely proud of this team for their commitment to making a difference in this patient’s life.”

Frank Papay, M.D., (center) directs Cleveland Clinic’s third face transplant. (DPSI Medical Photography)
When the Cleveland Clinic face transplant team reviewed this patient’s case, they had the end goal of face transplantation in mind – as facial reconstruction alone would not correct her facial disfigurement or improve her quality of life. With a face transplant at the forefront, the surgeons were able to safeguard any potential blood vessels that could be used for the transplant during her initial stages of reconstruction.
This surgery will give the patient the capability to speak more clearly, and breathe, chew, and swallow more effectively. She’ll also be able to use her face to better express emotions. In addition to significantly improved physical function, the patient will also have enhanced physiological, psychological and social function.
“Knowing this patient now has the opportunity to live a functional life because of her face transplant is the greatest reward,” said Dr. Gastman. “With a new nose, lips, palate, eyelids and jaw, she now has the full opportunity to re-integrate into society and have a future just like any other young adult. This surgery can give her back the self-esteem and confidence she lost.”
In a case of cooperative surgical innovation, the face transplant team utilized surgical rehearsal, 3-D printing and virtual reality as the main platforms for preoperative planning. These platforms helped optimize the accuracy, aesthetic and functional outcomes for the transplant.
Since the surgery, the patient is recovering well and getting accustomed to her new face. She is walking, talking and will begin eating orally shortly. She will continue to go through extensive rehabilitative therapy, including physical therapy, speech and swallowing therapy and occupational therapy. Doctors continue to monitor her closely for signs of tissue rejection. The patient, like all transplant patients, will remain on immunosuppressant medication for the rest of her life to prevent rejection.
In December 2008, Cleveland Clinic became the first U.S. hospital to perform a face transplant. At the time, it was considered the largest and most complex face transplant in the world, integrating different functional components such as nose and lower eyelids, as well as different tissue types including, skin, muscles, bony structures, arteries, veins and nerves.
Cleveland Clinic is one of six U.S. institutions that has conducted face transplants. Fewer than three dozen face transplants have been performed worldwide. This most recent face transplant was supported by the U.S. Department of Defense’s Armed Forces Institute of Regenerative Medicine I (AFIRM I) grant program. As an integral part of AFIRM, the Rutgers-Cleveland Clinic Consortium (RCCC) is committed to delivering advances in regenerative medicine that will improve the treatment of U.S. service members wounded on the battlefield. Through the RCCC, Dr. Siemionow – former director of Cleveland Clinic’s Department of Plastic Surgery Research – has served as the primary investigator of this clinical trial. Dr. Siemionow is now a professor of orthopedic surgery at the University of Illinois at Chicago College of Medicine and acted as a consultant and advisor on the recent surgery.

In a 31-hour surgery, a team of 11 Cleveland Clinic surgeons performed the hospital’s thrid face transplant. (DPSI Medical Photography)
With the creation of AFIRM in 2008, the U.S. government made a major investment to alleviate the suffering of patients in need of restorative therapies. Joachim Kohn, Ph.D., director of the RCCC of the AFIRM I and Board of Governors Professor at Rutgers, The State University of New Jersey, recognized the significant potential of Dr. Siemionow’s exercise in conducting face transplants and has been a strong advocate for the development of face transplant procedures. These extremely complex procedures are often the only treatment option left for patients with major facial deformities.
“I see this surgery as an important result of the investment made by the U.S. government aimed at advancing therapies for some of the nation’s most seriously injured patients,” said Dr. Kohn. “Considering the tremendous complexity of this surgical procedure, we had to cope with substantial challenges in the administration and management of this program. Dr. Sangya Varma, Ph.D., COO of RCCC and I established a strong collaboration with the administration and clinicians at Cleveland Clinic. This collaboration was effective in shepherding the AFIRM program to a successful conclusion. Looking ahead, the pioneering work done at Cleveland Clinic will contribute to making this important new treatment option available to other patients with devastating facial deformities.”
According to the U.S. Department of Defense, the U.S. Army Medical Research and Materiel Command supports efforts such as the Armed Forces Institute of Regenerative Medicine, which bring together leading scientists, clinicians, and industry partners to develop innovative medical solutions to restore service men and women to form, function, appearance and quality of life after traumatic injuries. Since 2009, the DoD has funded almost $60 million in hand and face transplant research, focusing on innovations offering immediate benefit to troops injured in combat and to civilians suffering traumatic injuries.
None of this would have been possible without the involvement of Lifebanc, Northeast Ohio’s nonprofit organization dedicated to saving and healing lives through organ, eye and tissue donation. The advancements of face and other vascular composite allograft (VCA) transplants offer new opportunities for healing. VCA donations, such as face, arms and uteri, are special requests with additional authorization above donations designated on the Ohio Donor Registry. The Lifebanc team works extremely closely with families of potential VCA donors to ensure that all their questions are answered and needs are met as they make the decision to allow these types of additional donations to occur.
“It was an honor for our team to work collaboratively with Cleveland Clinic on a case that will have such a profound impact on this patient’s life,” said Gordon Bowen, CEO, Lifebanc. “We are tremendously grateful to the donor and her family, with whom our team has developed a special bond during this process. It was the family’s decision to donate that has allowed this extraordinary miracle to occur and we are honored to continue to support them. We are appreciative of all those who commit to give the gift of life and healing. Designating one’s wishes can be done easily online in just moments, and the impact of giving more life is infinite.”
This work was supported by the Armed Forces Institute of Regenerative Medicine, under Award No. W81XWH-08-2-0034. The U.S. Army Medical Research and Materiel Command, Fort Detrick MD 21702-5014 is the awarding and administering acquisition office. Dr. Joachim Kohn is the Principal Investigator of the prime contract to Rutgers University. This work was conducted under a subcontract from Rutgers University to the Cleveland Clinic. Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the Department of Defense.





Sem comentários:
Enviar um comentário